Ontario Animal Health Network (OAHN) Companion Animal Network Team Public Health Update 2024
What is the OAHN Public Health Update?

The Ontario Animal Health Network (OAHN) was created to achieve coordinated preparedness, early detection, and response to animal disease in Ontario. OAHN is a “network of networks” with individual networks for different species/sectors, each of which involves collaboration among veterinarians, animal owners and stakeholders in the field with laboratory, academic and government experts. This annual update was created especially for public health professionals in Ontario, to highlight pertinent topics from the last 12 months from the OAHN companion animal and other species networks, to help strengthen the link and communication between animal health and public health networks.
Mpox in animals: Good news, bad news
In May 2022, an outbreak of mpox (formerly known as monkeypox) began, which ultimately resulted in over 87 000 human cases in 110 countries. Prior to this, this zoonotic disease occurred primarily in central and west Africa. Good news: A US study has just been released that tested 24 dogs, 9 cats and 1 rabbit from households with at least one human mpox case in 2022-2023. They found no evidence of infection in any of the pets, though some of the pets were contaminated with virus from the infected humans.
A new outbreak of mpox caused by the clade I MPX virus is now spreading in 2024, which differs from the clade IIb MPX virus that caused the 2022 mpox outbreak. Bad news: As we cannot be certain that the two clades will behave the same way in other species, so the same precautions as before are recommended for avoiding exposure of wild rodents especially, and for managing pets that may have been exposed to infected humans – basically, treat pets like any human member of the household by avoiding close contact as much as possible.
H5N1 flu: Cows & cats (S1 2024)
H5N1 highly pathogenic avian Influenza A (HPAI) continues to keep everyone on their toes. Since March, it has unexpectedly been found in dairy cattle in over 200 herds in at least 14 US states. While most dairy cattle appear to recover from infection with time and supportive care, cows shed large amounts of virus in their milk. Pasteurization effectively kills bacteria and viruses, including HPAI, so pasteurized products are safe to consume, but raw milk from infected cows is a risk, and has likely contributed to fatal H5N1 infections in barn cats fed raw milk on some of these dairies. This H5N1 flu has caused outbreaks in at least 29 species of mammals worldwide; in many of these (including cats) disease has often been fatal, but we still don’t know how often milder infections may occur in these species.
The risk of humans contracting the H5N1 influenza continues to be very low. Nonetheless, owners are encouraged to take appropriate precautions to protect their pets and themselves by avoiding direct and indirect contact with sick or dead wildlife, especially migratory birds. There are also precautions to take around livestock.
Ontario has only had two infected poultry premises since last summer, but there have been numerous detections in wild birds and one skunk (in Thunder Bay) this spring.
The companion animal and wildlife OAHN teams, along with CWHC, continue to collaborate on a joint pilot project on H5N1 influenza in primarily outdoor / feral cats. Visit the project webpage for details on case eligibility, sample collection and submission.
Other: Chlamydia caviae, guinea pigs (S2 2024)
In early summer 2024, many companion animal veterinarians reported young guinea pigs from commercial retail outlets in Ontario with bilaterial conjunctivitis, sometimes with respiratory signs. Given the likely common source, it is likely these guinea pigs had chlamydial conjunctivitis due to Chlamydia caviae.
An important differential for this condition in guinea pigs is infection with C. psittaci, the cause of psittacosis (also known as parrot fever) in people, which is often carried by psittacine birds. Chlamydia psittaci is notifiable to OMAFA, and notifiable to public health when it is found in birds. Guinea pigs are generally not capable of infecting humans with C. psittaci; C. caviae is a rare human zoonosis from exposure to infected guinea pigs. For more information, check out the OAHN C. caviae factsheet.
Update: Lyme disease infographic (S2 2024)
OAHN has once again updated its infographic for veterinarians on ticks and Lyme disease in Ontario with the latest risk area map for Ixodes spp. ticks from PHO. It also has quick tips on monitoring, screening, and when not to treat dogs. Also check out the OAHN tick checklist for pet owners!
Treat me right: Acute dog diarrhea (S3 2023)
Antimicrobial resistance and stewardship are critically important issues in veterinary medicine. As in human medicine, a key step to improving stewardship is reducing unnecessary (and ineffective) prescribing and use for common conditions. A systematic review and meta-analysis of antimicrobial and nutraceutical treatment of acute diarrhea in dogs (Scahill et al. 2023) was recently published. The main conclusions were that neither antimicrobials nor nutraceuticals (e.g. probiotics, fibre supplements) had a relevant clinical effect in these dogs in terms of duration of diarrhea or hospitalization, or progression of disease (to name a few). The certainty of the evidence with regard to antimicrobials was considered high in dogs with mild or moderate disease, but was low for dogs with severe disease.
The review was performed for the European Network for Optimization of Veterinary Antimicrobial Treatment (ENOVAT), which is expected to release new guidelines for acute diarrhea in dogs very soon. Diarrhea in dogs is unpleasant for everyone, but think twice before reaching (or asking) for antibiotics!
Raw meat-based diets infosheet (S1 2024)
Feeding raw meat-based diets (RMBDs) and/or raw treats such as bones, rawhides and pig ears carries clear risks to both pets and their owners, particularly infectious disease risks such as Salmonella and E.coli.
- Most recently this was illustrated by the 2020-2023 outbreak of XDR Salmonella in 6 provinces in Canada, including Ontario; the main risk factors for infection in people were exposure to raw pet food or dogs fed raw food.
Other risks of RMBDs include the potential for dietary / nutritional imbalances (especially in growing animals) and foreign body ingestion (e.g. swallowing bones). Despite many pet owner and company claims and anecdotal reports, there is little to no rigorous scientific data to support the alleged health benefits of feeding RMBDs compared to a properly balanced cooked commercial or homemade diet. So OAHN and Worms & Germs Blog collaborated to develop a Raw meat-based diets infosheet to help veterinarians talk to clients about the risk associated with these diets, and ways to mitigate them should the owner chose to feed a RMBD or raw treats.
Equine: Viral encephalitis cycle (S2 2024)
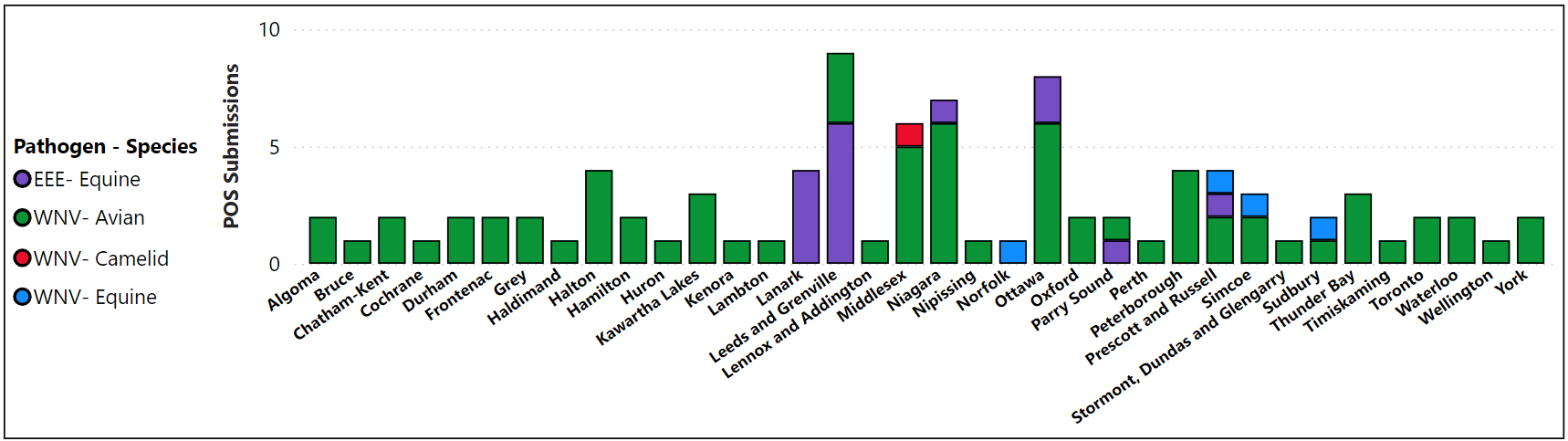
Eastern equine encephalitis (EEE) is an ever-present risk in certain geographical areas of Ontario. As for many diseases, viral encephalitides like EEE and West Nile (WN) tend to cycle over the years. So far in 2024 there have been 14 confirmed cases and at least as many additional suspect cases of EEE in horses throughout Eastern Ontario. Previous notable outbreaks of EEE include the same region in 2023, Parry Sound area in 2021 and Niagara region in 2018. These viruses cannot be transmitted directly by horses, but people and horses are infected the same way – via mosquitos – which also creates a seasonal pattern. Wild birds and horses are both important sentinels for disease risk in people, which can also be affected by climate change and warmer, wetter weather. Rabies is an important differential diagnosis in any horse with signs of acute encephalitis. More information on the occurrence of EEE, WN and other diseases in horses can be found on the interactive Ontario Equine Immediately Notifiable Disease Dashboard (2018-2024).
All species West Nile and EEE positive submissions (IgM and PCR) by location (2024 to 11-Sep).
Ruminant: Coxiella burnetii (Q fever) (S2 2024)
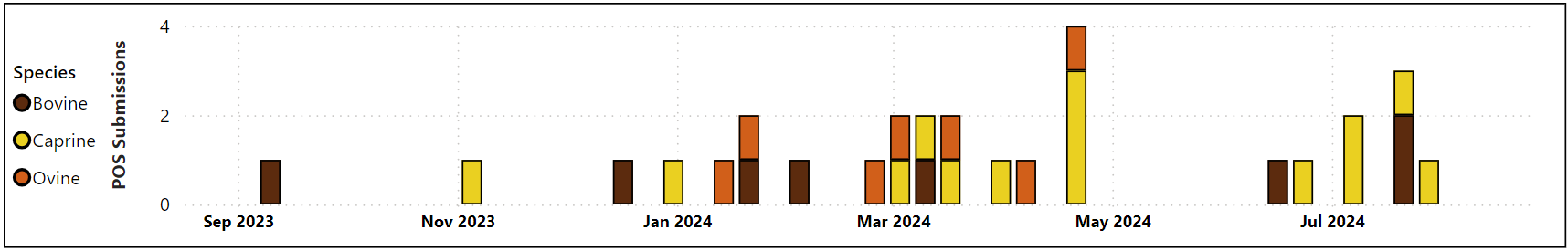
ICoxiella burnetii is a highly infectious zoonotic bacterium commonly found in domesticated and wild animals throughout the world, and is the cause of Q fever in humans. Coxiella burnetii in animals is immediately notifiable to OMAFA and trends are monitored by OAHN’s ruminant networks. It is in fact a relatively common finding in sheep, goats and cattle, and contact with these species always presents some risk of zoonotic transmission, especially around birthing. The graph below shows ruminant lab submissions positive for Coxiella (PCR & ELISA) Aug 2023-Aug 2024.
Survey: Anaplasma diagnosis & treatment (S3 2023)
In an effort to learn more about the situation with anaplasmosis in dogs and cats across Ontario, OAHN asked some questions about how often clinics are diagnosing exposure to this tick-borne pathogen and how they manage it:
- 86% of respondents reported the same or slightly increased numbers of seropositive dogs in 2023 compared to 2022, and 84% reported approximately the same number of dogs with suspected clinical anaplasmosis.
- 67% of respondents reported that for clinically normal seropositive dogs, they routinely run a complete blood count (CBC), which is the main recommendation in these cases. Of note, 10% of respondents reported that they routinely prescribe antimicrobials for these dogs; but antimicrobials are only recommended if the dog is clinically ill and/or has compatible changes on CBC.
- Clinical anaplamsosis in cats appears to remain rare (or rarely diagnosed) overall.
Anaplasma phagocytophilum was added to the list of periodically notifiable hazards in Ontario in February 2023, which will hopefully improve our ability to monitor trends in this disease over time.
Ontario seroprevalence maps for this and other tick-borne diseases (based on monthly data provided by Antech, IDEXX and Zoetis laboratories) are available on the Companion Animal Parasite Council website.
Changes to US dog import rules, AGAIN (S2 2024)
It has been a rollercoaster ride over the summer trying to determine what the new rules will be for dogs travelling to the US from different countries, including Canada. The first version of the rules was announced in May, followed by a number of changes in June and July ahead of the August 1 effective date, which included some detailed record requirements aimed at proving where the dog had been living for the last 6 months prior to entering the US. Then on July 22, the US CDC suddenly announced they were dramatically reducing the requirements for dogs coming from low-risk countries for dog-mediated rabies, like Canada. For now, all dogs must:
- Be at least 6 months old
- Have a microchip (readable by a universal scanner)
- Appear healthy on arrival
- Have a CDC Dog Import Form receipt
The requirement for a current rabies vaccination certificate for dogs coming from Canada has been dropped – for now. But remember that dogs returning to Canada will still require proof of current rabies vaccination, even if they have only visited the US. Canada’s Minister of Health (Hon. Mark Holland) confirmed that the US has agreed to a nine-month grace period while Canada and the US find a workable, permanent solution that will minimize disruption to Americans and Canadians crossing the border with their dogs. The CVMA has advocated for the involvement of both a CVMA and AVMA representative in future negotiations.
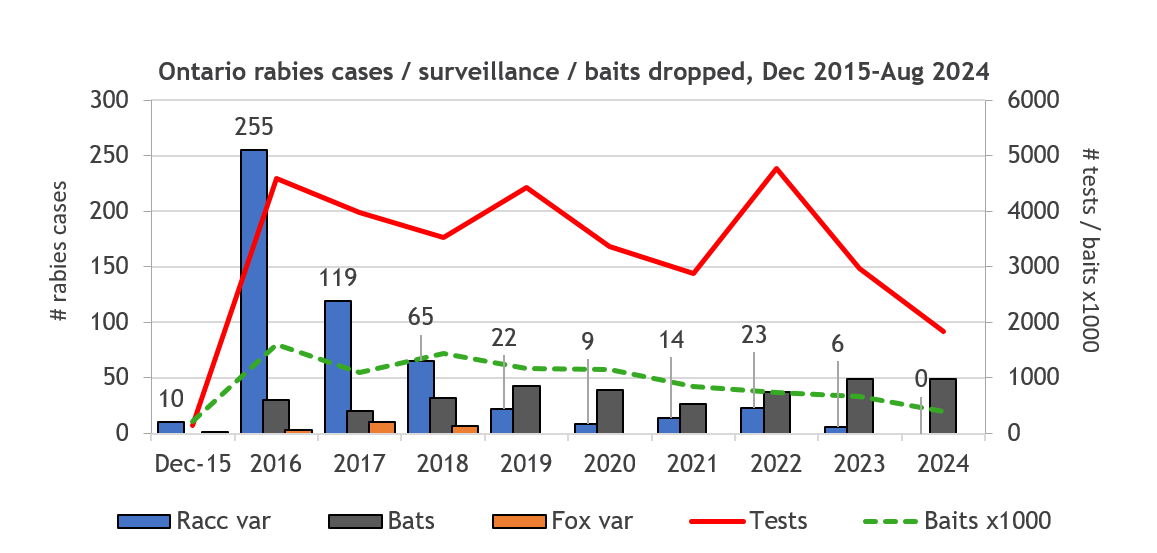
Wildlife rabies update
Rabies response and control in Ontario is a joint effort involving the public, animal owners, veterinarians, animal and wildlife control organizations, public health units, the Ontario Ministry of Agriculture, Food and Agribusiness (OMAFA) and the Ministry of Natural Resources (MNR). The MNR maintains an interactive Ontario rabies surveillance map and posts annual maps of rabies cases in Ontario (including terrestrial rabies and bat rabies cases). All raccoon-variant rabies cases since 2022 have been detected in the St. Catharines area. Rabies was also detected in a pet cat in St. Catharines in 2023, but the strain could not be typed. No cases have been detected in 2024 to date. Fox-variant rabies has not been detected in southern Ontario since 2018. The MNR’s 2024 rabies control operations are currently underway.
Bats: Beware but be kind!
Over 56 rabid bats have been detected in Ontario in 2024. Tragically, rabies was recently diagnosed in a person in Ontario who had contact with a bat in the province. ANY direct contact between a pet and a live bat is considered a potential rabies exposure, because bites are so difficult to detect in animals. Almost ALL dogs and cats – even if currently vaccinated – require a rabies booster within 7 days of a bat exposure, unless the bat can be tested (and is negative) within this window.
NEVER put a live bat in the freezer. Contacts for humane euthanasia of bats (and other animals for rabies testing) can be found on the OAVT Rabies Response Program (RRP) website. Also check out the new 1-page OAHN N2K: Bats in Ontario for more facts and tips on being kind to bats!
REMEMBER: Owners who have a concern about potential exposure of one of their animals to rabies should always be referred to their local veterinarian FIRST. Additional detailed rabies response information for veterinarians is available on Ontario Rabies: information for veterinarians page.
Not-so-tropical rat mite (S2 2024)
Mite infestations (aka mange) are quite common in many species, including pets like dogs, cats and rabbits. It is not always necessary to determine the type of mite involved, as most will respond to the same type of treatment. Sometimes when we look more closely, we find unexpected things, like one Toronto veterinarian who submitted samples for testing from a mangey rabbit that was infested with tropical rat mites (Ornithonyssus bacoti).
While they sound exotic, these mites are found globally in tropical and temperate regions, typically on wild rodents, but occasionally infecting managed breeding or research rodent colonies. Heavy infestations can cause anemia, alopecia and pruritis in animals. These mites are also zoonotic, causing rat mite dermatitis in people.
Rabbits are an unusual host for O. bacoti. The rabbit in this case was treated, but the finding pointed to a potentially significant rodent problem in the building where it lived, which was referred to the local public health unit for further investigation.
Animal surveillance who’s who (S1 2024)
Check out the new summary graphics about all the individuals and groups that contribute to disease surveillance in companion animals, horses and cattle in Ontario! Graphics for other species networks are in development.
IN THIS ISSUE
- What is the OAHN Public Health Update?
- Mpox in animals: Good news, bad news
- H5N1 flu: Cows & cats
(S1 2024) - Other: Chlamydia caviae, guinea pigs (S2 2024)
- Update: Lyme disease infographic (S2 2024)
- Treat me right:
Acute dog diarrhea(S3 2023) - Raw meat-based
diets infosheet (S1 2024)
- Antimicrobials in dogs and cats (S2 2024)
- Equine: Viral encephalitis cycle (S2 2024)
- Ruminant: Coxiella burnetii (Q fever) (S2 2024)
- Survey: Anaplasma diagnosis & treatment(S3 2023)
- Changes to US dog import rules, AGAIN (S2 2024)
- Wildlife rabies update
- Not-so-tropical rat mite (S2 2024)
- Animal surveillance who’s who (S1 2024)
USEFUL LINKS
NETWORK TEAM:
- Eastern ON:
Dr. Julie Calvert - Southern ON:
Dr. Emma Webster - Northern ON:
Dr. Hailey Bertrand - GTA ON
Dr. Donia Eino - Animal Health Lab:
Dr. Kris Ruotsalo
Dr. Emily Brouwer - Ontario Vet College:
Dr. Scott Weese
Dr. Shauna Blois
Dr. Allison Collier - OMAFA:
Dr. Maureen Anderson
Dr. Hannah Golightly - Network coordinator:
Dr. Tanya Rossi


